COMBINING SPECIALITIES
Team-working has been seen as an important essential in the delivery of modern medical care and quality, particularly in neurosurgery. With rapid development in newer techniques, and a better understanding of tumour biology there has been constant upgradation of neurosurgical services.
Neuro-anesthesia, neuro-radiology, neuro-pathology, neuro-oncology, and neuro-rehabilitation have become specialties by themselves. They all work together with the single aim of providing less risky, more beneficial, and long-term treatment options to patients.

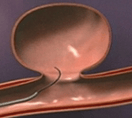
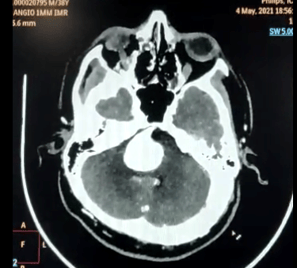
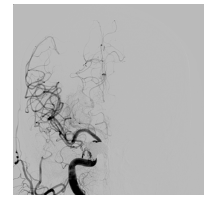
Coiling involves approaching the aneurysm from inside the blood vessel so that there is no need to open the skull. During endovascular coiling, a catheter is passed through the groin up into the artery containing the aneurysm. Platinum coils are then released. The coils induce clotting (embolization) of the aneurysm and, in this way, prevent blood from getting into it (and hence bleeding). The coils remain in the aneurysm; they are not removed.
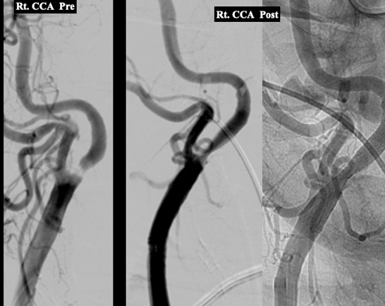
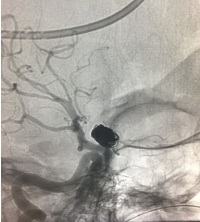
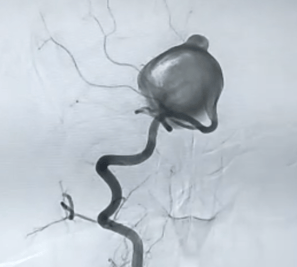
Below is an example of a Giant Aneurysm, which was treated by Dr Karapurkar, an interventional neuroradiologist and a neurosurgeon.
1.INTERVENTION NEURO-RADIOLOGY
It is a subspecialty of radiology, neurology, and neurosurgery. Interventional neuroradiologists currently employ minimally invasive procedures to accomplish a wide variety of treatments including stroke treatment by delivering clot-busting drugs directly to the site of the blockage, to open a stenosed blood vessel by angioplasty, aneurysm therapy by inserting platinum coils into the aneurysm sac, to name a few.
Aneurysm sac
a)ANEURYSM COILING
Done by Dr Nishant Aditya.
Giant Aneurysm
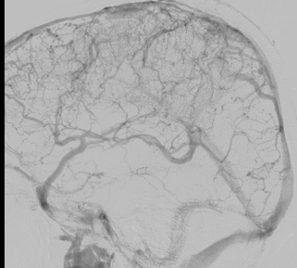
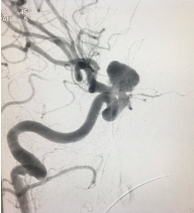
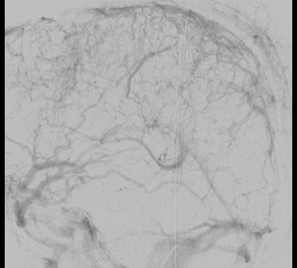
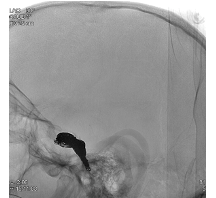
b)SSS THROMBOSIS
The superior sagittal sinus (SSS), also known as the superior longitudinal sinus is an unpaired large venous channel that drains blood from the lateral aspects of anterior cerebral hemispheres to the confluence of sinuses and ultimately to the heart. It is the major dural sinuses that receive a considerable amount of venous drainage of the brain.
It causes brain stroke and could be life-threatening.
A wide variety of diseases may be associated with thrombosis of SSS, including infectious diseases and non-infectious conditions such as vasculitis, hypercoagulable states like dehydration, and pregnancy, selected medications (e.g., oral contraceptives, substance abuse), and unpredictable events (e.g., head trauma).
It can be treated with anticoagulation even in the setting of intracranial haemorrhage (ICH) in most of the patients. In non-responsive cases, where the thrombosis is extensive, the patient may require endovascular treatment (thrombectomy) as shown below. This procedure is done by an interventional neuroradiologist.
Done by Dr Nishant Aditya.
Thrombosed SSS
After thrombectomy
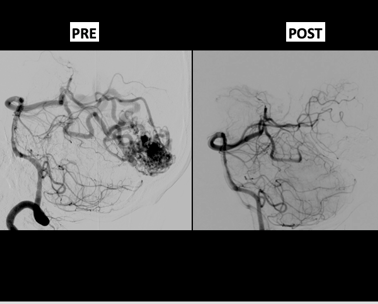
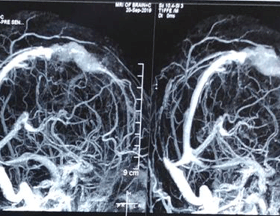
c)AVM EMBOLISATION
Cerebral arteriovenous malformations (AVMs) are complex high-flow lesions that can result in devastating neurological injury when they haemorrhage. Embolization is a critical component in the management of many patients with cerebral AVMs. Embolization may be used as an independent curative therapy or more commonly in an adjuvant fashion prior to either micro neurosurgery or radiosurgery.
ONYX A wide variety of agents have been used to embolize AVMs. Ethylene-vinyl alcohol copolymer (Onyx) is a more recently developed liquid embolic agent also used for the embolization of cerebral AVMs.
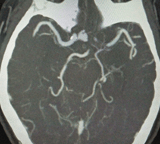
d)INTERNAL CAROTID ARTERY (ICA) STENOSIS
The carotid arteries are located on each side of your neck. These are the main arteries supplying blood to your brain. They can be clogged with fatty deposits (plaque) that slow or block blood flow to the brain, which can lead to a brain stroke. Carotid angioplasty and stenting are procedures that open clogged arteries to restore blood flow to the brain. They're often performed to treat or prevent strokes.
The procedure involves temporarily inserting and inflating a tiny balloon (angioplasty) into the clogged artery to widen the area so that blood can flow freely to your brain.
Carotid angioplasty is often combined with another procedure called stenting. Stenting involves placing a small metal coil (stent) in the clogged artery. The stent helps prop the artery open and decreases the chance of it narrowing again. Post-procedure, the patient is usually prescribed blood thinners or antiplatelet medicines for at least six months or longer to prevent blockage of the stent.
Done by Dr Nishant Aditya, an interventional neuroradiologist.
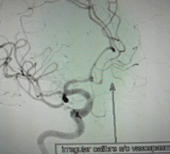
e)CHEMICAL ANGIOPLASTY FOR VASOSPASM
Cerebral vasospasm—the narrowing of the cerebral arteries after SAH—is a common complication that occurs in up to 70% of patients. Cerebral vasospasm may be present in some patients even in the first 24 hours of the precipitating event but more frequently begins 3 to 4 days after an aneurysm rupture, reaching a peak after 7 to 10 days and resolving spontaneously after 21 days.
Cerebral vasospasm leading to delayed cerebral ischemia (DCI) and dysfunction continues to be a major complication and source of morbidity in cases of aneurysmal SAH.
Various medicines are used to treat it. One of them is to inject a special drug (vasodilator) in the affected blood vessel. This is called chemical angioplasty.
Vasospasm
After IA Nimodipine
f)CAROTIDO-CAVERNOUS FISTULA
Post-traumatic carotid-cavernous fistulas are due to a tear in the wall of the cavernous carotid artery, leading to the shunting of blood into the cavernous sinus. These are generally high-flow fistulas and rarely resolve spontaneously. There is severe conjunctival congestion, haemorrhagic chemosis, ptosis (drooping of the eyelid), and pulsatile proptosis (bulging of the eyeball) accompanied by a whistling sound. If not treated promptly, it can cause loss of vision.
Most cases require endovascular embolization (disconnection of the fistula between the carotid artery and cavernous sinus).
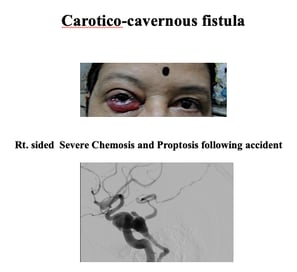

Fistula or abnormal communication
Blocking of the fistula with coils
Done by Dr Nishant Aditya, an interventional neuroradiologist.


Done by Dr Nishant Aditya.
Giant Aneurysm
Done by Dr Nishant Aditya.
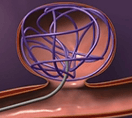
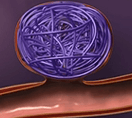
Packing of aneurysm sac with coils









2.STEREOTACTIC RADIOSURGERY
Radiosurgery is surgery using radiation, that is, the destruction of precisely selected areas of tissue using ionizing radiation rather than excision with a blade. It is not surgery in the traditional sense because there is no incision. Like other forms of radiation therapy (also called radiotherapy), it is usually used to treat cancer and many other benign conditions.
It is often a safer alternative to standard brain surgery (neurosurgery), which requires incisions in the scalp, an opening in the skull and membranes surrounding the brain, and dissection into brain tissue. This type of radiation treatment is usually performed when a tumour or other abnormality in the brain is difficult to reach with standard neurosurgery or for a residual tumour (after surgical excision), or if the patient isn't healthy enough to undergo standard surgery, or if he or she prefers a less invasive treatment.
Apart from malignant tumours, it is used to treat small (less than 2.5 cm) benign brain tumours, trigeminal neuralgia, AVMs, to name a few.
Residual tumour after surgery, treated with Radiosurgery

3.NEUROPATHOLOGY (Molecular Biology and targeted therapy)
Neuropathology is the study of diseases of the eyes and of the nervous system, which includes the: Brain. Spinal cord. Neuropathologists are increasingly becoming part of research teams looking into neurological diseases such as brain tumor's, Alzheimer’s, Huntingdon’s and Parkinson’s, etc.
Until recently, diagnostics of brain tumours were almost solely based on morphology and immunohistochemical staining for relatively unspecific lineage markers.
Molecular biology is one such field, where the genetic study of the tumour (tumour markers) is done. Molecular markers are fragments of DNA, which are genetic signatures for discovering alterations in gene sequences, expression levels, and protein structures or functions. Genomics provides a comprehensive study of cancer, which helps in the molecular characterization of the tumours. Based on gene expression studies tumours that used to be considered single entities so far, can now be grouped and can be treated differently (targeted therapy).
Targeted therapy toward specific genetic tumour alterations is still of limited use in the treatment of CNS tumours. Hopefully, future research will enable the development of new drugs that specifically target the genetic alterations that drive the progression of these aggressive tumours, thereby improving survival and quality of life.
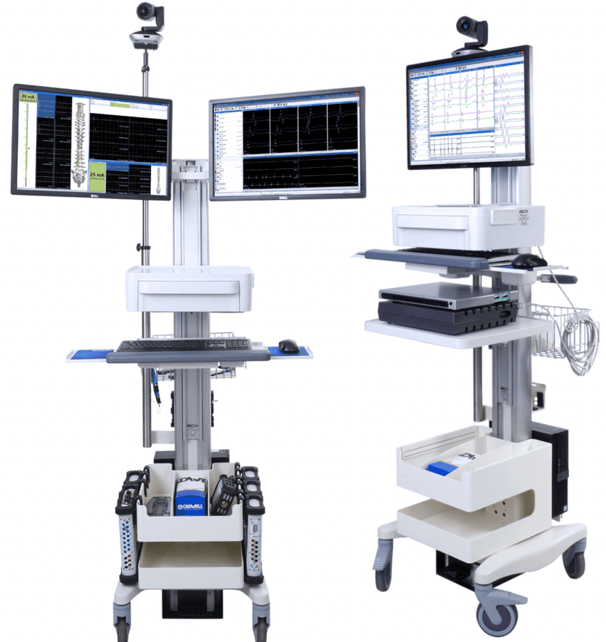
4.TECHNOLOGICAL SUPPORT
Apart from rapid developments in diagnostics and intensive care units, the following are the technologies useful to do safer neurosurgery.
1. Neuro navigation
2. Microscope
3. CUSA
4. IONM
Neuro navigation
Neuro-Microscope
CUSA
IONM