VASCULAR
1.LARGE CEREBRAL ARTERIO VENOUS MALFORMATION (AVM)
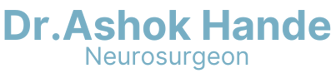
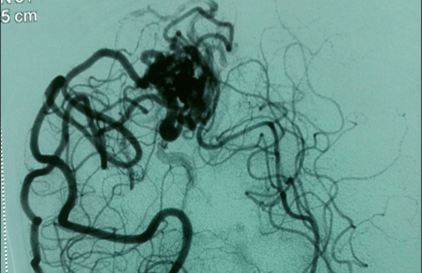
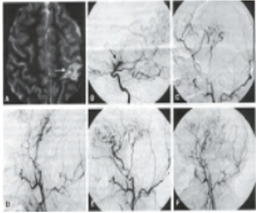
This 23-year-old college-going student presented with repeated episodes of convulsions. The MRI scan of the brain raised suspicion of an AVM. There was no brain hemorrhage. The cerebral angiography showed a large AVM. This was symbolised by my neuroradiologist colleague. The residual AVM was later excised completely by microsurgical techniques. The patient made an uneventful recovery without any neurological recovery. However, his anticonvulsant medicines continued.

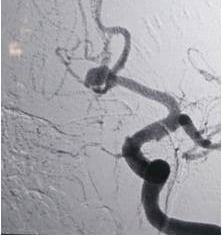
DSA-Before surgery

During surgery
2.CEREBRAL ANEURYSM
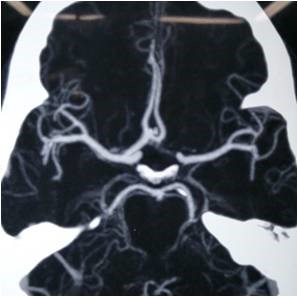
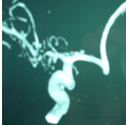
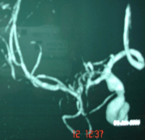
Aneurysm is a balloon on the blood vessel. Many times, it is discovered after it ruptures, causing brain haemorrhage, or subarachnoid haemorrhage (SAH). Occasionally, it is an incidental finding. This haemorrhage can be life-threatening and needs immediate treatment. It is diagnosed either by CT angiogram or by Digital subtraction angiography (DSA).
CT angiogram
Digital subtraction angiography (DSA).
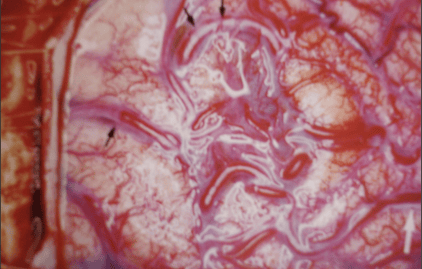
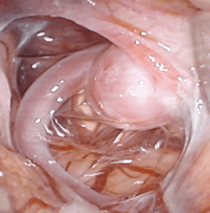
This 45-year-old lady presented with a brain hemorrhage. The cerebral angiography showed a large aneurysm of the middle cerebral artery. The aneurysm was clipped successfully. She made an uneventful recovery. We always use an endoscope during these surgical procedures to confirm complete occlusion of the aneurysm and to exclude occlusion of any other blood vessel.
ANEURYSM SURGERY- INTRAOP PICTURE






3. REVASCULARISATION PROCEDURES FOR TIA
A. Encephalo-duro-arterio-synangiosis(EDAS)
Transient ischemic attack (TIA) and minor ischemic stroke are associated with brain dysfunction due to regional reduction in blood flow (ie, ischemia), resulting in transient clinical symptoms. Identification of ischemia is important as 20% of patients with ischemic stroke present with a TIA in the hours to days preceding the stroke. Up to 80% of strokes after TIA are preventable; thus, early diagnosis and treatment are key. Encephaloduroarteriosynangiosis (EDAS), which involves the transposition of a segment of a scalp artery onto the surface of the brain, is a surgical treatment aimed at improving collateral blood flow.
Generally, it is advocated in children with Moya Moya disease, but has shown promising early results in the treatment of adult patients with Moyamoya disease (MMD) and more recently in patients with intracranial atherosclerotic steno-occlusive disease. The rates of stroke after EDAS are lower than those reported with other treatments, including intensive medical therapy in patients with TIA.
CT and MRI are the recommended modality to diagnose TIA and image ischemic lesions. In addition, Transcranial Doppler sonography (TCD) and Digital Subtraction Angiography (DSA) are two acceptable alternatives for diagnosing TIA patients.
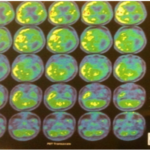
PET imaging can be used to quantify areas of altered cerebral blood flow and abnormal glucose and oxygen metabolism. This can be used to elucidate areas of ischemic penumbra and infarcted tissue. It is used as an imaging biomarker to detect high-risk carotid plaques.
PET CT before surgery
PET CT 6 months after surgery
B. STA-MCA Anastomosis Surgery
Direct revascularization (STA-MCA bypass) involves the use of a branch of a scalp artery (STA) for direct anastomosis (connection) to a branch of the brain artery (MCA) on the outer surface of the brain. This procedure benefits patients by providing an immediate improvement in blood supply to the brain.
This can be done as a stand-alone procedure or can be combined with the EDAS procedure.
Stenosis of the artery
After STA MCA Anastomosis
C. Carotid Endarterectomy
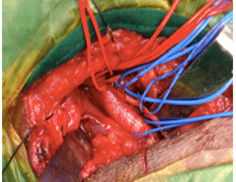
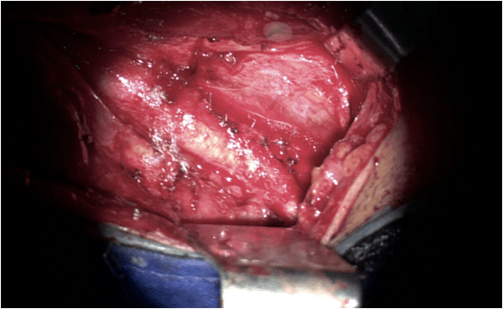
A carotid endarterectomy is an open procedure where one or both of your carotid arteries become narrowed because of a build-up of fatty deposits (plaque). This is known as carotid artery disease or carotid artery stenosis, and it significantly increases your risk of having a stroke or transient ischaemic attack (TIA). It could be a medical emergency and needs immediate attention. This 30-year-old patient presented with transient limb weakness. He had suffered from a similar episode 3 years ago, from which he had improved significantly. He was non-diabetic but was hypertensive and a heavy smoker. MRI with MR angiography, cerebral angiography, and carotid showed a large floating thrombus in the internal carotid artery at its origin.
Thrombus
Thrombus No Flow
Thrombus removed. Flow resumed
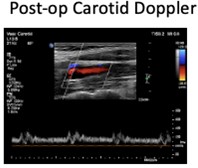
SURGERY: He underwent an emergency open carotid endarterectomy with excellent postoperative recovery. His limb weakness has not recurred or deteriorated since then.
DSA in a TIA patient
Carotid exposure in the neck
After Carotid Resuring














4.CAROTID STENTING
This is another way of treating carotid stenosis by intervention neuro-radiology.
This 46 year old patient presented with repeated episodes of giddiness and transient limb weakness (called transient Ischemic attacks). He was hypertensive, diabetic, and a heavy smoker. The carotid angiography showed severe stenosis of the internal carotid artery at its origin causing compromise of brain circulation. The patient preferred carotid stenting over open surgery.
Following successful carotid stenting by our interventional neuroradiologist, the patient made an uneventful recovery. His symptoms disappeared completely. In addition, he needed a complete change in his lifestyle.
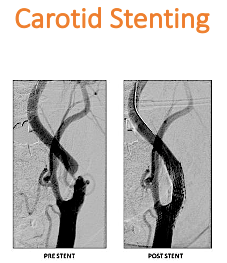

Done by Dr Nishant Aditya