MENINGIOMA
A meningioma is a tumour that forms on membranes that cover the brain and spinal cord just inside the skull. Specifically, the tumour forms on the three layers of membranes that are called meninges. These tumours are often slow-growing. As many as 90% are benign (not cancerous).
It isn't clear what causes a meningioma. Radiation therapy, female hormones, and genetics may play a role. In most cases, the condition is non-cancerous. Symptoms depend on the size of the tumour, changes in vision, headaches, hearing loss, and seizures. A small, slow-growing meningioma that isn't causing signs or symptoms may not require treatment. When required, treatment might involve surgery or radiation. Surgery to treat a meningioma is a complex procedure that is not without certain risks and complications. These are very vascular tumours, there can be considerable blood loss during surgery. They can invade important structures, making them difficult to excise completely. It is then wiser to leave some tumour behind and follow their growth by MRI.
1. LARGE FALCINE MENINGIOMA- MASSIVE BLOOD LOSS
Meningiomas are highly vascular brain neoplasms that are often associated with substantial blood loss during surgical resection. Sometimes. Blocking of the blood supply (Embolization) to the tumours can be a preoperative adjuvant therapy that has proved to be particularly effective in mitigating blood loss during surgical resection. These are called angiomatous meningiomas. Angiomatous meningioma is a rare and distinct variant of meningioma and accounts for 2.1% of meningiomas. Gross total resection is the treatment of choice for angiomatous meningioma. Postoperative radiotherapy may help the patients with residual tumour. Angiomatous meningiomas belong to WHO grade I and has a favorable prognosis, The completeness of surgical resection is the single most important factor in deciding prognosis.
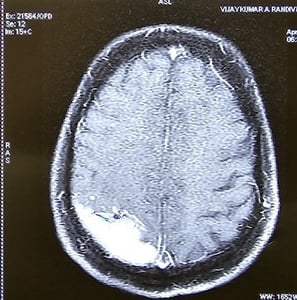
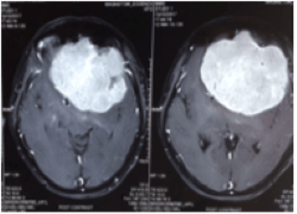
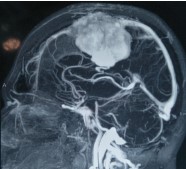
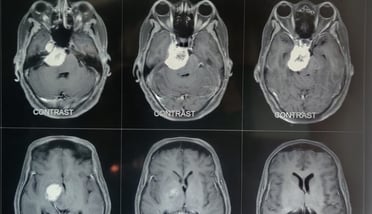
Giant highly Vascular Meningioma
Total tumour excision - post operative CT Scan
Patient after surgery (with permission)




2.LARGE MENINGIOMA INFILTRATING THE SUPERIOR SAGITTAL SINUS (SSS)
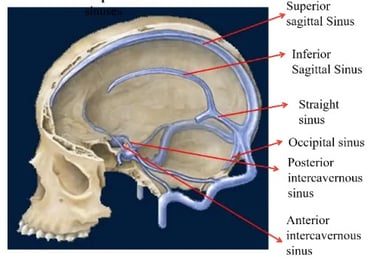
Dural venous sinuses are a group of sinuses or blood channels that drains venous blood circulating from the cranial cavity. The dural venous sinuses lie between the periosteal and meningeal layers of the dura mater. They are best thought of as collecting pools of blood, which drain the central nervous system, the face, and the scalp. All the dural venous sinuses ultimately drain into the internal jugular vein and then to the heart. Since meningiomas arise from the dura mater, sometimes the tumour can invade these dural sinuses making total tumour excision difficult.
Brain
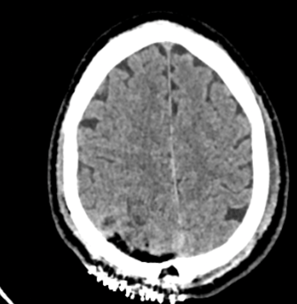
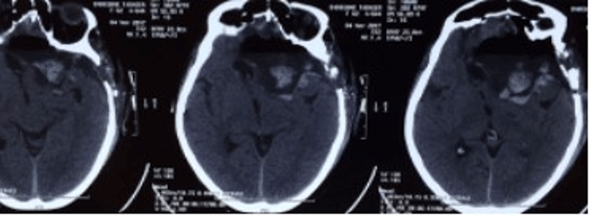
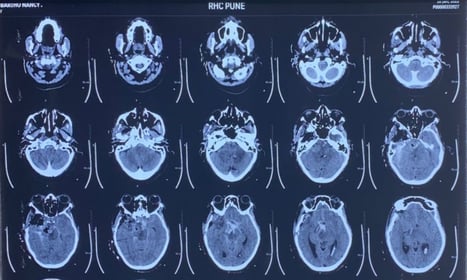
Giant meningioma in the midline infiltrating SSS
This tumour infiltrated the major dural venous sinus
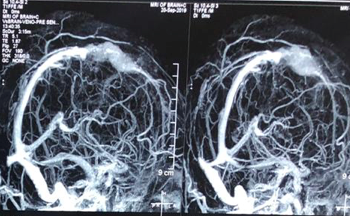
MRI Venogram after surgery showing Small Residual Tumour which was treated with Radiosurgery



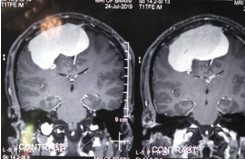

Surgical treatment of meningiomas next to venous sinuses is difficult because of their irregular growth patterns and infiltration into the venous sinuses, making gross total resection impossible in some patients. Radical resection of meningiomas invading the major dural sinuses remains controversial.
If the sinus is incompletely occluded or the adjacent drainage vein could not be dissected from tumour, subtotal resection of the tumour followed by SRS may be a good alternative treatment option.
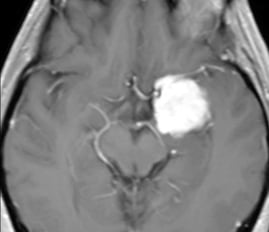
3.ANTERIOR CLINOIDAL MENINGIOMA (ACM)
Visual loss is a very common presenting symptom in these tumours, since they are situated just above the optic nerve. The characteristic onset usually occurs with unilateral failure of vision loss associated with primary optic atrophy. In some patients, loss of vision may extend to the opposite eye. Visual field defects in the form of concentric narrowing of the visual field, central scotoma, and temporal hemianopsia can be seen in patients; however, the extent depends on the degree of the involvement of the chiasm and the optic nerves. Headache is another most common symptom in these tumours, generally over the orbital or retroorbital field.
Clinoidal meningiomas remain a challenging pathology because of their intimate relationship to vital neurovascular structures, like optic nerves, and internal carotid artery, to name a few.
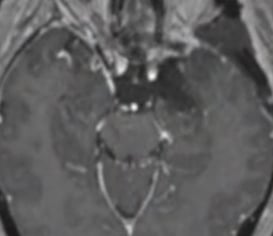
MRI-After surgery
Patient-After surgery (with permission)
MRI-Before surgery






4.PETROCLIVAL MENINGIOMA (PCM)
Petroclival meningioma is a benign and slow-growing tumour that occurs deep within the centre of the skull base, which is a very difficult location to reach surgically. Patients may experience headaches, double vision, hearing loss, dizziness, facial pain or numbness, facial weakness, and loss of coordination.
Petroclival meningiomas are regarded as probably the most difficult tumour to be treated by microsurgery. Frequent tight brain stem adherence as well as encasement of the basilar artery, its perforators and cranial nerves adds to the sometimes extreme difficulties of surgical tumour removal.
The treatment modalities considered in such tumours are microsurgery alone, microsurgery and adjuvant radiosurgery, though microsurgery is the primary treatment.
Large petroclival meningioma
CT Scan - Before surgery
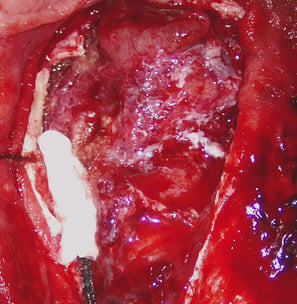
Partial tumour removal during surgery


5.MOTOR STRIP MENINGIOMA
These tumors has property to invade the brain coverings and known to grow inside the brain tissues unlike other meningiomas. Despite the small size these are difficult tumors as surgery can damage underlying brain and the blood vessels.
Invasive motor strip meningioma
During Surgery
CT Scan-After surgery